Health Desk
Sandeep Dhand
Nutritionist And Health Educator
Introduction to Bone Diseases
Bones are living tissues that provide strength, structure, and support to the body. They protect internal organs, store minerals like calcium and phosphorus, and produce blood cells in the bone marrow. However, like other body organs, bones can also suffer from several diseases caused by infections, metabolic imbalances, hormonal problems, cancers, and genetic disorders.
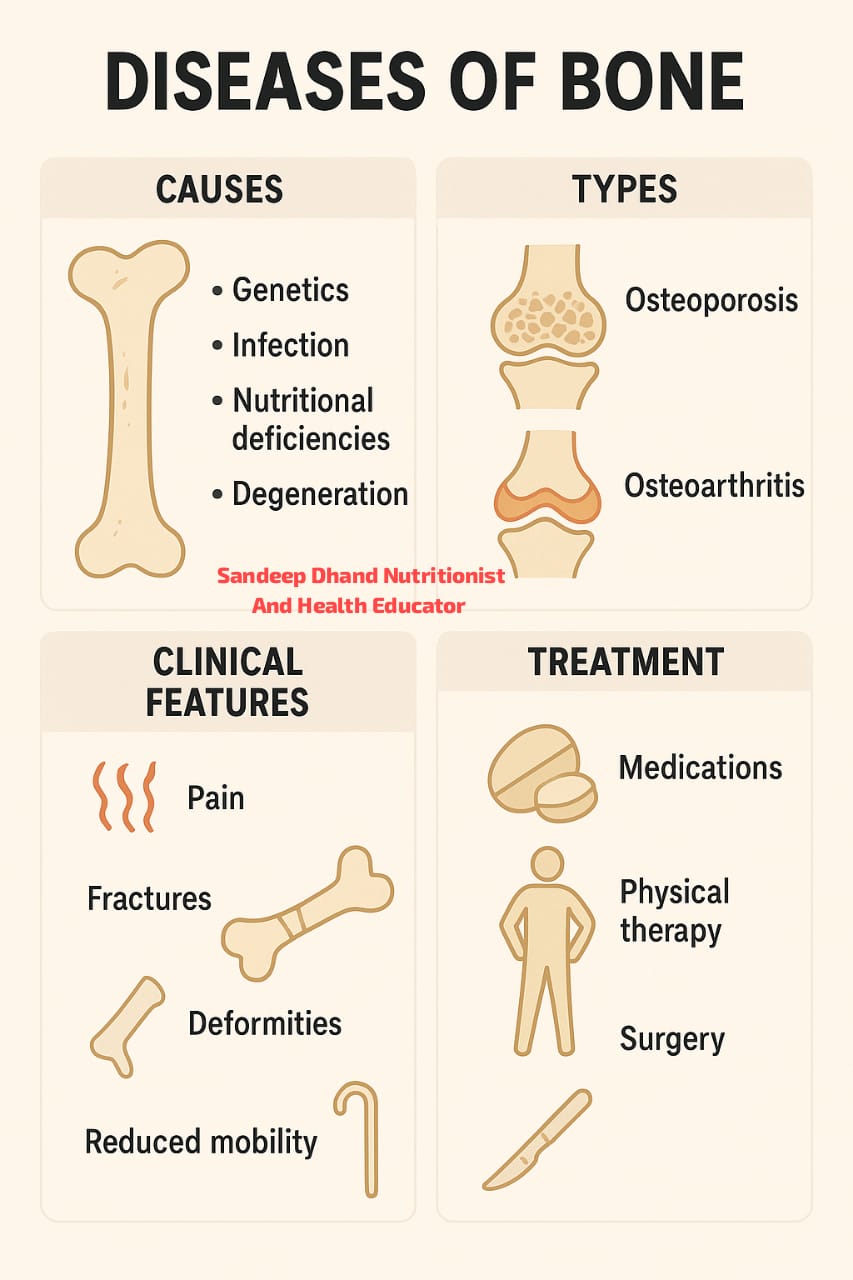
Bone diseases may cause pain, deformity, weakness, fractures, and in severe cases, disability. Understanding these conditions helps in early detection, proper treatment, and maintaining healthy bones throughout life.
In this article, we will explore different types of bone diseases including infections, Paget’s disease, metabolic and endocrine disorders, neoplastic (tumor) diseases, and skeletal dysplasia. We will also discuss their clinical features, diagnosis, treatment, and the future prospects in rheumatology.
Bone Infections (Osteomyelitis)
What Is a Bone Infection?
Bone infection, medically known as osteomyelitis, is caused by bacteria or fungi invading the bone. It can occur through the bloodstream, from nearby tissues, or after a fracture or surgery. The most common bacteria responsible is Staphylococcus aureus.
Types of Osteomyelitis
- Acute Osteomyelitis – develops suddenly, usually in children.
- Chronic Osteomyelitis – long-standing infection that may lead to bone destruction.
- Hematogenous Osteomyelitis – infection spreads through blood from another part of the body.
- Contiguous Osteomyelitis – occurs after injury, surgery, or ulcers (especially in diabetics).
Symptoms
Severe bone pain and tenderness
Swelling and redness over the affected area
Fever, fatigue, and chills
Difficulty in moving nearby joints
Pus discharge or sinus formation (in chronic cases)
Diagnosis
Blood tests showing raised white blood cells and ESR
X-rays or MRI showing bone damage
Bone biopsy or culture to detect bacteria
CT scan for detailed imaging
Treatment
Antibiotics: Long-term course (4–6 weeks) based on the type of bacteria.
Surgery: To remove dead bone tissue (debridement).
Drainage: To remove pus or abscess.
Supportive Care: Rest, immobilization, and proper nutrition.
If untreated, osteomyelitis can cause chronic pain, bone deformity, or even amputation.
Paget’s Disease of Bone
Overview
Paget’s disease is a chronic bone disorder where normal bone remodeling is disrupted. Old bone breaks down faster than usual, and new bone forms in an abnormal shape — larger but weaker and deformed. It mostly affects older adults.
Commonly Affected Areas
Skull
Spine
Pelvis
Long bones of legs
Causes
Exact cause unknown
Possible genetic link (family history)
Viral infections in bone cells (suspected in some cases)
Symptoms
Bone pain and deformity
Enlarged skull causing hearing loss or headaches
Bowing of legs
Back pain due to spinal involvement
Increased risk of fractures
Diagnosis
Blood Test: Elevated alkaline phosphatase levels.
X-rays: Show thickened and deformed bones.
Bone Scan: Detects multiple affected sites.
Treatment
Medications:
Bisphosphonates (like Alendronate) to control bone turnover.
Calcitonin to reduce bone pain and activity.
Pain Management: NSAIDs for relief.
Physical Therapy: To maintain mobility.
Surgery: For fractures, deformity correction, or joint replacement if required.
With proper treatment, most people can live normal lives with Paget’s disease.
Metabolic and Endocrine Bone Disorders
These are bone diseases caused by disturbances in mineral metabolism or hormonal imbalance.
A. Osteoporosis
A condition where bones become weak and brittle due to loss of calcium and minerals.
Causes: Aging, menopause, lack of vitamin D, sedentary lifestyle, corticosteroid use.
Symptoms: Fractures, back pain, stooped posture, height loss.
Treatment: Calcium and vitamin D supplements, weight-bearing exercise, bisphosphonates.
B. Osteomalacia and Rickets
These occur due to vitamin D deficiency.
Rickets: In children, leads to bowed legs and skeletal deformities.
Osteomalacia: In adults, causes soft bones and muscle weakness.
Treatment: Vitamin D-rich diet, sunlight exposure, supplements.
C. Hyperparathyroidism
Excess parathyroid hormone causes calcium loss from bones, making them fragile.
Symptoms: Bone pain, kidney stones, fatigue.
Treatment: Surgery to remove the overactive gland, calcium control.
D. Hypoparathyroidism
Low parathyroid hormone leads to low calcium, causing muscle cramps and brittle bones.
Treatment: Calcium and vitamin D supplements.
E. Thyroid Disorders
Hyperthyroidism: Increases bone loss leading to osteoporosis.
Hypothyroidism: May cause joint stiffness and slow bone growth.
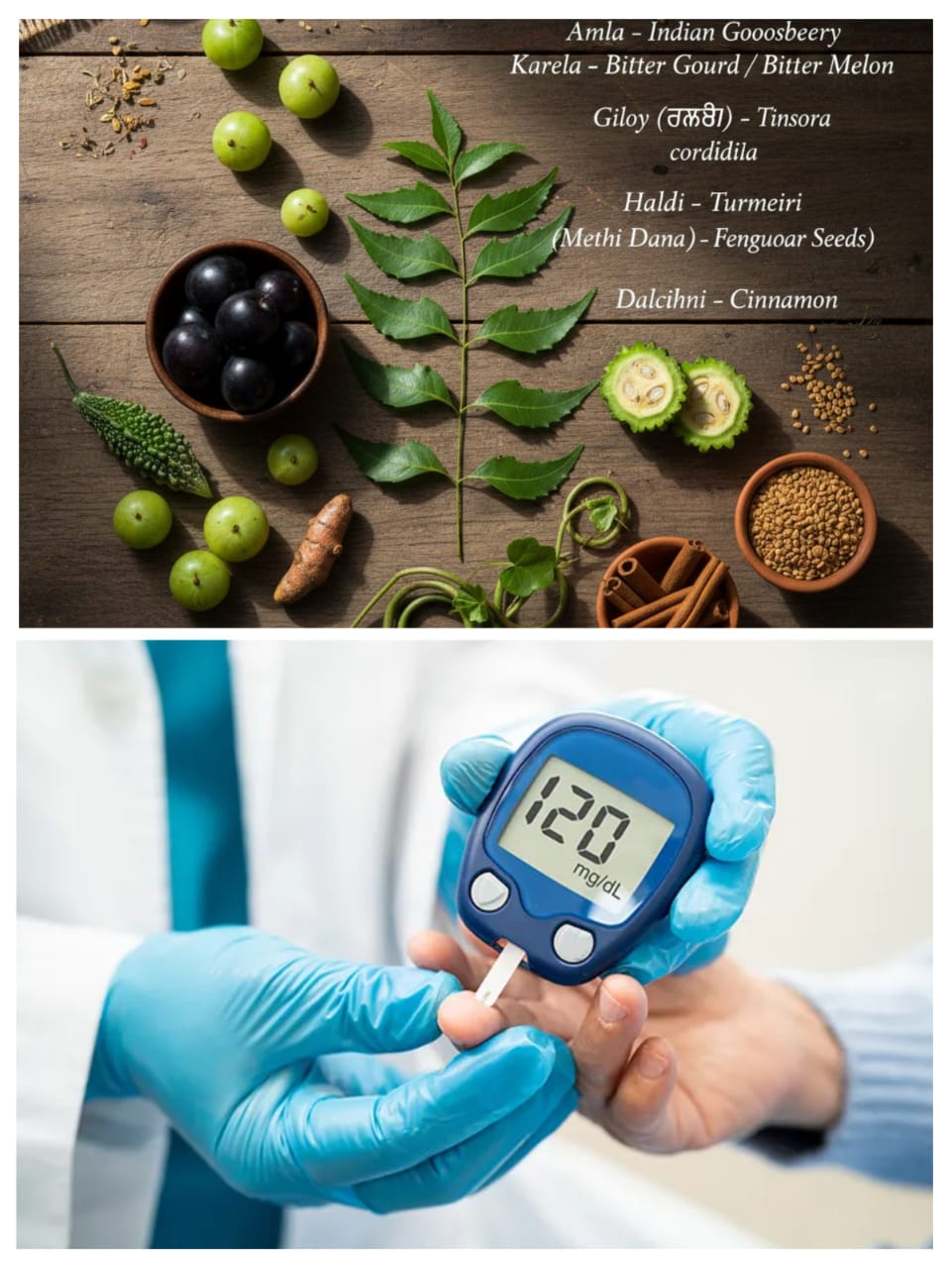
F. Diabetes and Bone Health
Chronic diabetes affects bone density and healing. Maintaining good blood sugar levels supports bone strength.
Neoplastic Diseases of Bone (Bone Tumors)
What Are Bone Tumors?
Neoplastic diseases refer to abnormal growth of bone cells forming benign (non-cancerous) or malignant (cancerous) tumors.
A. Benign Bone Tumors
These grow slowly and rarely spread.
Common types include:
Osteochondroma
Osteoid Osteoma
Giant Cell Tumor
Enchondroma
Symptoms: Mild pain, swelling, and deformity.
Treatment: Surgical removal if painful or growing.
B. Malignant Bone Tumors
These are cancerous and may spread to other organs.
Common types include:
Osteosarcoma – common in teenagers, affects long bones.
Chondrosarcoma – arises from cartilage, mostly in adults.
Ewing’s Sarcoma – affects children and young adults.
Metastatic Bone Cancer – spreads from other organs (like breast, lung, prostate).
Symptoms:
Severe bone pain
Swelling and lump formation
Fractures with minor injury
Weight loss, fatigue
Diagnosis:
X-rays, MRI, CT scans
Bone biopsy
Blood and bone marrow tests
Treatment:
Surgery to remove tumor
Chemotherapy and radiation
Pain management and physical therapy
Early diagnosis improves survival in bone cancers.
Skeletal Dysplasia
Definition
Skeletal dysplasia refers to a group of genetic disorders affecting bone and cartilage growth. It leads to short stature, abnormal bone shape, and joint deformities.
Common Types
- Achondroplasia – short limbs with normal torso.
- Osteogenesis Imperfecta – brittle bone disease causing frequent fractures.
- Thanatophoric Dysplasia – severe form leading to stillbirth or early death.
- Multiple Epiphyseal Dysplasia – abnormal joint development causing pain and arthritis.
Symptoms
Short height or dwarfism
Deformity of spine, arms, or legs
Joint stiffness
Bone fragility
Hearing or vision problems (in some types)
Diagnosis
Genetic testing
X-rays of bones
Family history
Prenatal screening in some cases
Treatment
No complete cure; focus is on improving quality of life.
Physical therapy, orthopedic surgery, and growth hormone therapy (in some cases).
Counseling and support for affected families.
Clinical Features of Bone Diseases
While each bone disease has unique symptoms, some general signs include:
Bone Pain: Constant or movement-related pain.
Swelling and Redness: Around joints or affected bones.
Deformity: Bowed legs, curved spine, or enlarged bones.
Fractures: Recurrent or with minor trauma.
Restricted Movement: Stiffness or joint limitation.
General Symptoms: Fatigue, fever, weight loss (in infection or cancer).
Diagnosis and Investigations
Accurate diagnosis requires a combination of medical history, physical examination, and investigations:
- Blood Tests:
Calcium, phosphorus, vitamin D levels.
Alkaline phosphatase for bone activity.
ESR and CRP for infection.
- Imaging:
X-rays for structure and fracture.
CT/MRI for detailed imaging.
Bone scan for metabolic activity.
- Bone Biopsy: Confirms infection or cancer.
- Genetic Tests: For inherited bone disorders.
Treatment and Management
General Management
Rest and immobilization in acute cases.
Physical therapy for recovery.
Balanced diet with calcium, vitamin D, protein, and minerals.
Sunlight exposure for vitamin D synthesis.
Regular exercise to maintain bone strength.
Medical Treatment
Antibiotics for infection.
Bisphosphonates for Paget’s disease and osteoporosis.
Hormonal therapy for endocrine disorders.
Chemotherapy and radiation for cancers.
Pain relief and anti-inflammatory drugs for comfort.
Surgical Management
Debridement for infected bones.
Fixation for fractures.
Joint or bone replacement in severe damage.
Removal of tumors or bone grafting when needed.
Diet and Lifestyle for Bone Health
Calcium-Rich Foods: Milk, cheese, curd, ragi, tofu, almonds.
Vitamin D Sources: Sunlight, fortified foods, eggs, fish (for non-vegetarians).
Protein: Pulses, beans, soy products, lean meat.
Avoid: Smoking, alcohol, excessive salt or caffeine.
Exercise: Weight-bearing exercises like walking, jogging, and yoga strengthen bones.
Prospects in Rheumatology
Rheumatology deals with diseases of joints, bones, and connective tissues. Modern research is bringing hope for better diagnosis and treatment of bone diseases.
Future Developments
Stem Cell Therapy: For bone regeneration.
Gene Therapy: Targeting genetic bone disorders.
Biologic Drugs: To control inflammation and bone destruction in arthritis.
Advanced Imaging: For early detection of bone loss or cancer.
3D Printing of Bones: For surgical reconstruction.
Rheumatology is rapidly evolving, and with new scientific advancements, patients with bone diseases can expect better outcomes, less pain, and improved quality of life.
Conclusion
Bone diseases range from simple infections to complex cancers and genetic disorders. Early diagnosis, proper nutrition, and timely medical treatment can prevent serious complications. Maintaining a healthy lifestyle, regular checkups, and bone-friendly habits are key to lifelong bone strength.
Understanding these disorders helps healthcare professionals and individuals recognize early symptoms and seek appropriate care. With continuous progress in rheumatology and bone research, the future of bone health looks promising — aiming for stronger, pain-free lives for millions of people worldwide.